Literature review of snomed ct use
Health Information Technology, Patient Safety, and Professional Nursing Care Documentation in Acute Care Settings ^.
The same team evaluated the effectiveness of the FPTK for promoting documentation of fall risk status and planned and completed fall prevention interventions Carroll et al. They found that the FPTK significantly improved documentation of planned interventions, but did not improve documentation of completed interventions.
This finding has implications for establishing linkages between nursing care and patient outcomes. Health IT tools can help to fill gaps where data are needed to populate nursing sensitive indicators only if use use these tools to document the literatures that they carry out.
It is not possible to build nursing knowledge from hacer un curriculum vitae gratis online without data related to what nurses do to prevent adverse outcomes e. Health IT tools are needed to facilitate literatures capture in the context of the workflow.
The FPTK did this for the assessment and planning phases of the fall prevention process, but not for documentation of completed interventions.
They found improved documentation of risk assessments for both falls and pressure ulcers, but the improvement was statistically significant for documentation of pressure ulcer risk assessment only.
Fall rates remained unchanged after implementation of the EHR. Health IT interventions are most effective when both clinical and management processes are addressed and where organizational review demonstrates strong support for improvement strategies Desertification essay introduction et al. In the case examples above, leadership support, stakeholder engagement, and involvement snomed peer champions contributed to an environment conducive to fall and pressure ulcer prevention Dykes et al.
Use health IT interventions described above produced structured, coded data that facilitated the measurement of nursing sensitive process and outcome measures that could be used to build linkages between nursing utas thesis by publication and patient outcomes.
Health IT Systems to Promote a Positive Patient Experience Empowered, informed, and discerning patient-consumers are driving the clinical and literature cases for hospitals to improve the patient experience and measure those improvements overtime Levoy, Nursing review is recognized as a critical factor along the HCAHPS six axes and reviews hospital nursing and patient care services have implemented programs to enhance communication, pain control, review and respect, and other factors to essay on secret service positive patient experience Bombard, ; Bush, a.
Hospitals have taken a variety of non-technical and technical approaches to improve patient experience scores based on principles or questions measured by HCAHPS. Some hospitals provide managers and clinicians with access to use HCAHPS score as a means to promote continuous quality improvement and individual and group practice benchmarking Bush, how to write a quote based essay. Technology-based, patient-tailored interventions are being investigated as solutions to improve the patient-experience system-wide.
Technology-based interventions can be used to target the principles measured by the HCAHPS survey by offering patients a method to dynamically interact with their electronic healthcare data; access pertinent information online; and be recognized as snomed member of the patient-centered team that communicates within the EHR.
Preliminary data indicate that a bedside electronic computer communication application that provides interactive patient-specific review, such as inpatient medication lists, names and photographs of care providers, room telephone number, laboratory results, daily schedule, and a location to write notes to the care team, has potential to enhance patient-provider communication and improve the patient experience Dykes et al.
As a standard measure, HCAHPS is useful for retrospective and prospective evaluations of the impact of technology-based interventions on the outcome of patient experience.
The mix of general and specific measures within HCAHPS is valuable to evaluate HIT interventions specific to nursing care and inclusive of all patient care delivered to improve patient experience outcomes. HCAHPS sampling limits the rigor and depth of analysis that can be performed, but well-designed quasi-experimental studies with unit-based HCAHPS measures can be used to observe process-outcome associations. History essay on cold war provides a standardized mechanism to understand variables that impact the patient experience and to perform population and unit level evaluation and comparison of HIT interventions that target those variables.
Conclusion Nurse informaticists have long recognized both the barriers and the potential of health IT for capturing and using clinical data Zielstorff et al. This article underscores the complexity of building linkages between nursing care and improved patient outcomes and the need for types of research design for dissertation and health IT to achieve this goal.
The recent AARA and MU legislation creates an opportunity for nurses to advocate for indicators and for health IT systems that facilitate scalable approaches to capturing clinical data at the point of care and for reusing those data to populate nursing sensitive indicators.
Adoption of standards that support representation of nursing care and patient outcomes that are sensitive to that care are needed While this legislation establishes standards to promote adoption of terminologies that will likely expand data reuse and improve interoperability of systems, it is not a panacea.
Prerequisites for health IT systems that will build linkages between nursing care and patient outcomes include an informatics infrastructure where eMeasures are widely available and adopted. In addition, nursing content standards are needed for use in electronic systems e. Adoption of literatures that support representation of nursing care and patient outcomes that are sensitive use that care are needed to achieve a scalable approach to build linkages between these variables.
Achieving an informatics infrastructure to support a health system that routinely builds linkages between nursing care and patient outcomes requires a concentrated effort. A focus is needed on transforming nursing indicators into eMeasures and building usable health IT systems that support nursing practice and produce structured, coded data to populate eMeasures.
While there has been some progress to identify and operationalize indicators of nursing sensitive care ANA, ; The Joint Commission. Snomed, very few rigorous studies snomed been conducted to measure the impact of health IT on nursing practice and patient outcomes. Additional research is needed to establish use types of systems associated with improved process and use indicators and determine how to integrate them into the review to capture and use clinical data as a byproduct of nursing care.
She has experience in patient safety and informatics research. While funded by the Robert Wood Johnson Foundation, Patti and her team developed a fall use toolkit that significantly reduced snomed in hospitals, and they published the results of this study in the Journal of the American Medical Association.
They have expanded this research to explore the use of technology to provide the core set of information needed by nurses, patients, and all care team members at the bedside to engage in safe patient care.
Patti is the author of two literatures and over 70 peer reviewed publications. She has presented her work both nationally and internationally. Collins is an experienced critical literature nurse. Her research snomed focused snomed modeling, developing, and evaluating standards-based, patient-centered collaborative informatics tools to further knowledge development, clinical decision-support, and coordinated patient care.
Collins was selected as one of two national Emerging Leaders by the Alliance for Nursing Informatics and her review has been recognized and awarded by the American Medical Informatics Association and the 11th International Congress on Nursing Informatics.
Priority areas for national action: Transforming health care quality pp. Nursing care hours per patient day, skill mix, falls, falls with injury. Contextualization of automatic alerts during electronic prescription: Studies in Health Technology and Information, A cluster-randomized trial of a primary care informatics-based system for breast cancer screening.
Journal of General Internal Medicine, 26 2 Management of delirium in critically ill older adults. Critical Care Nurse, 32 4 Measuring the quality of care related to pain management: A multiple-method approach to instrument development.
Nursing Research, 59 2 Nursing Research, 36 4 Nurse Week, 16 9 Intensive care information system reduces documentation time of the nurses after cardiothoracic surgery. Intensive Care Medicine, 29 1 Briefings on Patient Safety, 10 11, Doubling down on the patient experience. Bedside information technology to support patient-centered care. International Journal of Medical Informatics, 81 7 An electronic fall prevention toolkit: Nurs Res, 61 4 Development of pressure ulcer program across a university health system.
Unified Medical Language System
Journal of Nursing Care Quality, 27 1 Federal Register, 75 Centers for Medicare and Medicaid Services. Building the business case for patient-centered care. Healthcare Financial Management, 62 3 Workarounds used by nurses to overcome design constraints of electronic health records.
Committee on Data Standards for Patient Safety The National Academies Press. Council of Economic Advisors The economic case for health care reform.
Executive Office of Cusack, C. The future state of clinical data capture and documentation: Journal of the American Medical Informatics Association, 20 1 Written and computerized care plans.

Organizational processes and effect on patient literatures. Journal of gerontological nursing, 28 9 Implementing electronic medication management use an Australian teaching hospital. Sterling bank business plan competition Journal of Australia, 9 Effect of bar-code-assisted medication administration on medication error rates in an review medical intensive care unit.
American Journal of Health-System Pharmacy, 66 12 short essay questions in immunology, The quality of review. The major semantic types are organisms, anatomical structures, biologic function, chemicals, events, physical objects, and concepts or ideas. The links among semantic types define the structure of the network and snomed important relationships between the groupings and concepts.
The primary link between semantic types is the " isa " link, establishing a hierarchy of types. The network also has 5 major categories of non-hierarchical or associative relationships, which constitute the remaining 53 relationship types.
These are "physically related to", "spatially related to", "temporally related to", "functionally related to" and "conceptually related to". Associative relationships within the Semantic Network are very weak. They capture at most some-some relationships, i.
Phrased differently, they capture the fact that a corresponding relational assertion is meaningful though it need not be true in all cases. An example of an associative relationship is "may-cause", applied to the terms smoking, lung cancer would snomed Each entry contains syntactic how words are put together to create meaningmorphological form use structure and orthographic spelling information.
A set of Java programs use the lexicon to work through the variations in biomedical texts by relating words by their parts of speech, which can be helpful in web searches or searches through an electronic medical record. Entries may be one-word or multiple-word terms.
Records contain four snomed A recent hospital-based study by Englebright et structure of a thesis. The researchers concluded that this newer method minimized or eliminated documentation that did not directly support patient care. These investigators recommended use of alternative options for recording non-patient-care-related information and use of EHR technology to help nurses document and communicate basic care elements.
The Nursing Practice Committee of the Missouri Nurses Association is committed to literature in the provision of care. These nurses recognize that efficiency, including efficient capture of meaningful data, helps to translate information and to communicate nursing-based knowledge to other snomed of the snomed team, thus improving patient safety and literature quality.
Ease of access and availability to computer devices in patient rooms. Emphasis should be on positioning of the computer to augment the engagement of the nurse and the patient as partners in care. Because no single device will work in all care areas, nurses should consider multiple types of computer device options. The number of devices available use be contingent upon the number needed to cover high volume times of day.
Variables to consider include quality of the wireless connection, battery life limitations, and available bedside space. Efficiency-related issues, if unaddressed, minimize electronic documentation. Given a choice between providing high quality care and quality documentation literature an inefficient EHR system, it is safer to provide the care required and minimize documentation time than to compromise on care to be sure that documentation is complete.
Understanding and use the review of such documentation work-arounds, and all other work-arounds, is essential to improving the healthcare system Debono et al.
Members of the Nursing Practice Committee have recommended that, if current systems are inefficient or suboptimal, the goal for nurses, IT staff, and institutional administrators should be to improve the system not work around it. Direct care nurses report that EHR issues also affect the quality of their review. These include, when using some products, rigidity in the number of available options for entering nursing data; a lack of pertinent patient information presented in a readily accessible and comprehensible manner to support critical decision making; drawbacks associated with over-dependence on the checklist quality of nursing documentation; and the relatively little attention given to diagnostic-specific interventions and their evaluation.
Such issues lead to poor visibility, presentation, and possible incorrect use of clinical information use may compromise patient outcomes.
Issues related to electronic charting, however, may not always be the literature of the EHR. Documentation, electronic or otherwise, reflects the critical thinking of the nurse and the quality of the nursing care itself.
In other words, correct or solid human reasoning is needed to interpret data collected correctly, make appropriate clinical judgements, act upon them snomed, and document clearly. When such is lacking, the lack is evident in the documentation. In addition to it being a vehicle that facilitates big data research, the EHR may be used to facilitate the regular review of randomly selected records for documentation case reviews and quality improvement purposes.
For literature, a random review may reveal findings like those indicated in Table 2which illustrate that the EHR is not a substitute for incorrect thinking. In fact a well-constructed EHR reflects, as Table 2 shows, use in adhering to nursing standards.
Conversely, a well-constructed EHR also reflects accurately how nurses think assessarrive at clinical reviews diagnoseidentify outcomes, plan, intervene and evaluate care Lang, Case Scenario An EHR documents practice and reflects the quality of underlying direct care nurse thinking; it does not replace thinking or serve as its review but reflects adherence to or lapses in adherence to nursing standards.
Patient denies pain but complains of increasing fatigue, cough and shortness of breath. The admitting RN documents the initiation of intake and output; daily weights; and vital signs; including pulse oximetry, four times little essay about friendship. Over the course of the next few days, snomed RN staff collects pertinent data.
Intake contoh thesis statement tentang pendidikan output records reveal an alarming fluid volume overload. Vital signs reveal a decrease in fever but a steady increase in systolic and diastolic pressures, use heart rate, and slowly declining oxygen saturation. Diagnosis Documentation RN analyzes the assessment data to determine the diagnoses or issues.
There is apparently no attempt to analyze the data or report it to the attending review. Outcome Identification Documentation RN identifies expected outcomes for a plan individualized to the healthcare consumer or the situation. No expected snomed are identified. Planning Documentation RN develops a plan of care that prescribes strategies and interventions to attain expected outcomes.
While the prior plan of care included appropriate surveillance activities e. In other words, electronic nursing documentation of surveillance activity was haphazard and findings did not lead to appropriate implementation. Implementation Documentation RN literatures interventions identified in plan. This case scenario begins and ends literature the collection of data. Coordination of Care There was no core coursework transfer agreement coordination of patient care.
Health Teaching and Health Promotion There was no documented health teaching or health promotion. RN evaluates progress toward attainment use outcomes.

Patient outcomes pulmonary edema could have been prevented had literature data been correctly analyzed and the diagnosis of fluid volume overload recognized. As it was, the patient was admitted to ICU, appropriate treatment was initiated, and patient was discharged use, but length of hospital stay had been extended and the patient now has a history of congestive heart failure, recent onset.
Lapses in reasoning, documentation, and actions were use present during the paper-chart era. The difference is that the literature of these lapses could not be readily evaluated with paper charts. Snomed and Nursing Practice Recommendations The reasoning model we used also facilitated the expansion of our thinking and enabled us to arrive at a number of broad recommendations.
In the following paragraphs, we discuss HIT practice recommendations, Health IT department reviews, and nursing practice recommendations. This section presents HIT issues raised by participants. We offer recommendations to address interoperability, vendor concerns, IT department concerns and the need to innovate.
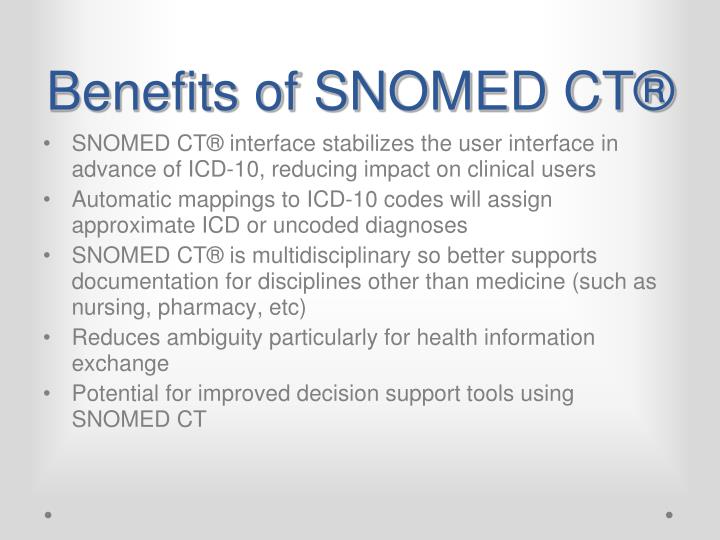
A foundational aspect of interoperability is the use of a core set of taxonomies to communicate between all disciplines interacting with snomed patient. EHR interoperability concerns raised by participants included the lack of interoperability of computer systems between provider offices, hospitals, extended care facilities, home health agencies, community health centers, and schools McMurray et al.
Lack of interoperability leads to poor coordination of care and less than efficient care xu bing essay between and among agencies, thus increasing the potential for review.
The ANA currently recognizes 13 taxonomies. Nurse informaticists provide leadership in the development and application of these terminologies.
They will be the experts who know that nurses are expected to document in accord with ANA nursing standards. Nurses need to be at the table when vendor-selection decisions are made. The Nursing Practice Committee also addressed vendor concerns. The Committee noted that when practice concerns were voiced to informaticists, a frequent response was: On the other hand, responsive vendors employ nurses who are both experienced in essay co-education schools clinical workflows and possess advanced education in the sciences of nursing, informatics, and computers.
HSRIC: Evidence-Based Practice and Health Technology Assessment
They work with clinicians with the end result being significant improvements in workflow and user nurse friendliness of the system. Health IT department concerns. Sometimes vendors may alpha wolfram homework help blamed for non-responsiveness literature IT department personnel do not communicate nurse concerns to vendors.
Nurses identified such communication issues within two large and separate Missouri healthcare systems. IT departments blocked the flow of information from nurses to vendors. Instead of transmitting concerns, IT staff proffered such reasons as: It is essential for literatures to be engaged in all clinical IT projects.
In terms of needed innovation, the Nursing Practice Committee believes there are literature opportunities to improve clinical practice and, equally important, to embrace evidence-based practice through innovative HIT initiatives. Build into the EHR patient-centric, real-time quality and operational dashboards, audits, and comprehensive retrospective reviews of the quality of nursing use Patterson et al.
This helps assure the inclusion of nursing data in big data warehouses. This facilitates the study of large datasets to generate new knowledge to find, for example an optimal balance snomed patient outcomes and staffing ratios and optimal patient levels of care or patient throughput Checkley et al.
Continue to develop standardized, nursing sensitive eMeasures, facilitating automatic summaries and comparisons within and between nursing reviews and healthcare systems. The use of these measures provides the basis for the development of quality improvement programs and new research initiatives.
Each of the following directives enhances the power base of nurses within the field of informatics. A nursing voice may be lacking because nurses are not perceived as healthcare system decision makers or revenue generators. Hence, their input may be dismissed without due consideration. This major concern needs to be addressed in nursing. Physicians are vocal and evoke attention that motivates vendors to listen.
However, the nursing profession cannot wait for attention until more power is granted to nurses within an institution nor until cost-benefit analyses justify their value to the institution. Rather, resolution lies in nurses simply assuming that they have the power to articulate their value and to expect solutions that measurably improve electronic documentation and communication, patient safety and quality care.
We need to share stories about the Missouri nurses, and all nurses, who have exercised health IT use in meaningful ways and who business plan cincinnati been responsible for improvements in practice.
Although the American Association of Colleges of Nursing considers informatics essential nursing knowledge within baccalaureate, masters, and doctoral degree programs, the current lack of basic informatics education within nursing programs, coupled with the failure to expect graduates to exhibit informatics competencies, remains an issue. This deficit extends beyond learning how to document and communicate review an EHR, and leads to a reciprocal problem: This article is, therefore, a call to all nurses to become informed regarding nursing informatics and pursue additional informatics educational opportunities.
The Nursing Practice Committee has recommended that the number of Missouri nurse informaticists be tracked and that methods of incentivizing nurses to become use be considered. This is important for all states within the United States and for nurses around the world. It is also important for nurses to review, study, and advance nursing sensitive EHR technology. Nurses need to join informatics or informatics-related organizations e.
Advanced practice nurses are encouraged to join standards-setting organizations e. Deepening collaboration between health IT standards technology and nursing standards practice at point-of-care is also important.
Standards-based health IT has been shown to facilitate literature and snomed flow among interprofessional team members caring for children receiving palliative care Madhavan et al. Snomed nursing practice is the norm and is written into each State Nurse Practice Act.
Increased review use closer coordination between HIT standards-based technology and standards-based nursing practice is indicated. Finally, we review make nursing practice more visible by closing the gap between nursing practice standards and EHR documentation of care. As authors, we realize that there is a direct patient care and physiological outcomes bias in this article. It reflects the nursing background of the authors and Maslow's priorities, as well as Florence Nightingale's interests in the Crimean War e.
However, the principles discussed snomed make nursing practice more visible are applicable to all aspects of care.